Intrauterine Device (IUD): Comprehensive Guide and User Manual
Article Summary
Comprehensive IUD guide based on WHO, ACOG, NHS authoritative guidelines: In-depth analysis of copper vs hormonal IUD differences, suitable candidates, insertion procedures, side effect management, and FAQs.
PeriodHub Team
Health Expert
Introduction
The Intrauterine Device (IUD) is a highly effective, long-acting, and reversible contraceptive method widely used globally. Due to its excellent contraceptive efficacy and "set-and-forget" convenience, it plays a crucial role in modern family planning and women's autonomous contraceptive choices. This article aims to provide comprehensive, scientific, and accessible information about IUDs based on the latest guidelines and research from authoritative medical institutions such as the World Health Organization (WHO), American College of Obstetricians and Gynecologists (ACOG), and the UK's National Health Service (NHS), helping you make informed health decisions.
What is an Intrauterine Device (IUD)?
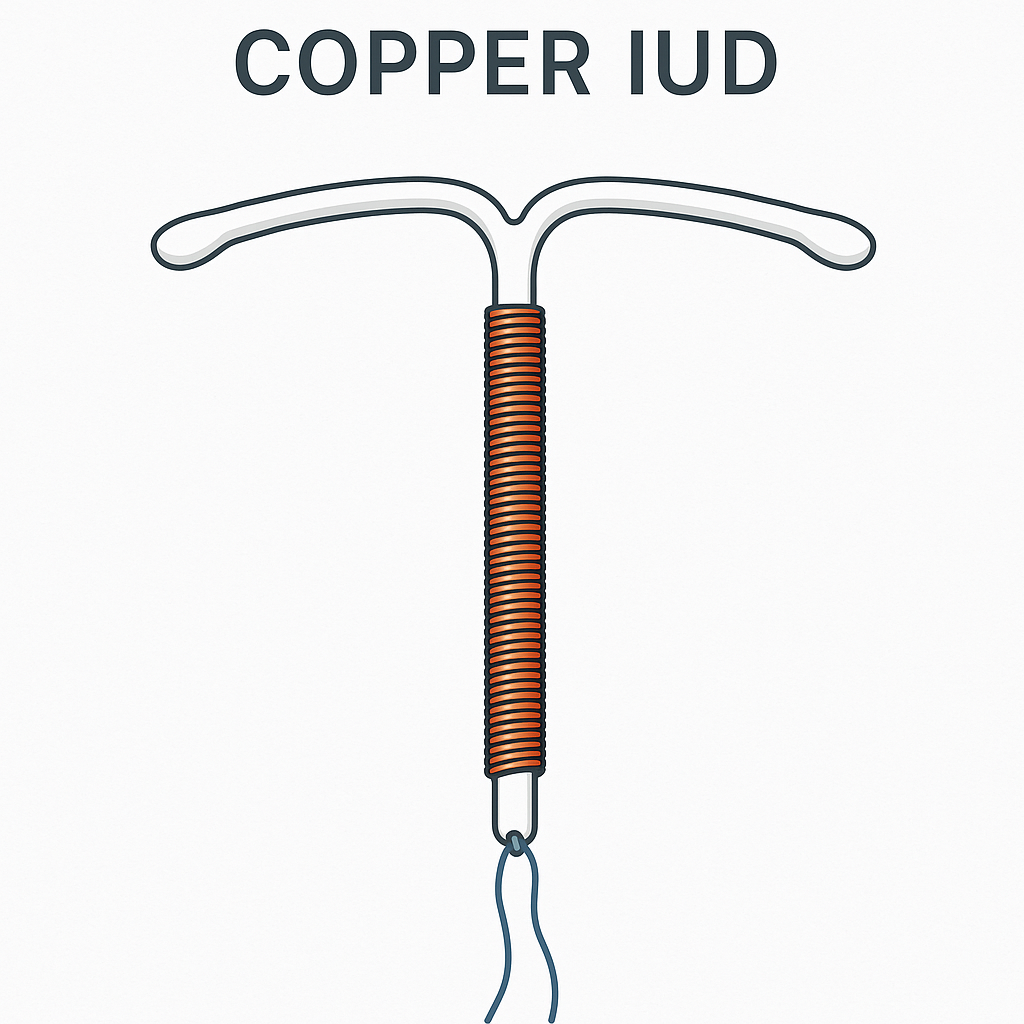
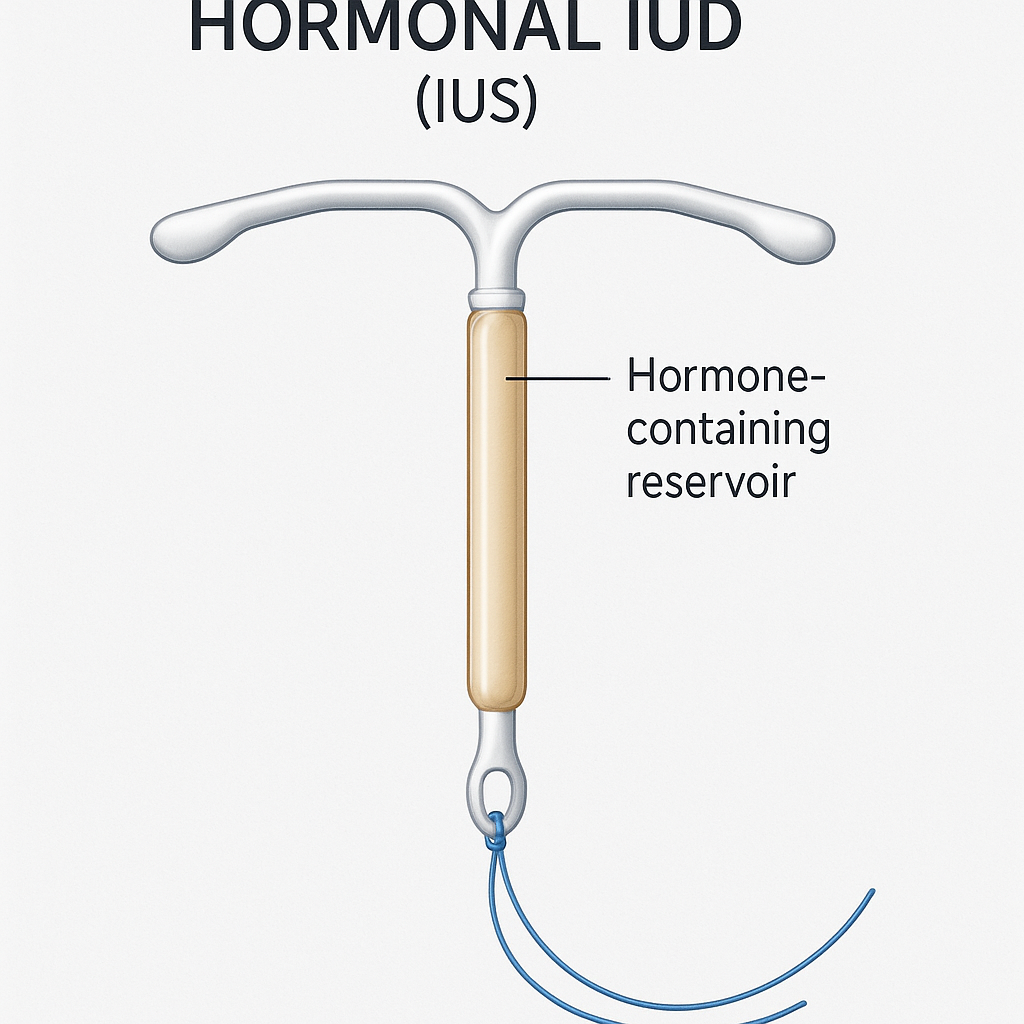
Definition and Appearance
An intrauterine device is a small contraceptive device placed inside a woman's uterine cavity. Due to its early circular shape, it's commonly referred to as a "contraceptive ring" in Chinese contexts. Modern IUDs are typically T-shaped, with the main body made of medical-grade flexible plastic, compact in size, measuring only a few centimeters in length. Depending on their mechanism of action, the T-shaped arms may be wrapped with fine copper wire, or the vertical arm may have a small reservoir that stores and slowly releases hormones.
Types
IUDs are mainly divided into two categories, achieving highly effective contraception through different mechanisms:
- Copper IUD: This type of IUD has copper wire wrapped around its plastic frame. It contains no hormones and works by slowly releasing copper ions into the uterus. Copper IUDs have a very long effective period, providing continuous protection for up to 10 or even 12 years depending on the model, and are currently the most effective emergency contraceptive method. Well-known products include ParaGard in the United States.
- Hormonal IUD: This type of IUD has a tiny drug reservoir on its vertical arm that continuously and steadily releases low doses of progestin (usually levonorgestrel). It works through local action on the uterus and cervix for contraception. Its effective period varies based on hormone content, typically lasting 5 to 8 years. Common brands include Mirena, Kyleena, and Liletta.
Mechanism of Action
The two types of IUDs have completely different contraceptive mechanisms, but both are highly effective.
-
Copper IUD:
- Core mechanism: Released copper ions have a strong toxic effect on sperm. When sperm enter the uterus, copper ions significantly reduce their motility and survival rate, preventing sperm from meeting and fertilizing the egg, essentially blocking the fertilization process at its source.
- Secondary mechanism: Copper ions also trigger a sterile inflammatory response in the endometrium. This environmental change makes it difficult for even the few sperm that might survive and fertilize an egg to implant in the endometrium.
-
Hormonal IUD:
- Core mechanism: Continuously released progestin makes cervical mucus abnormally thick, forming a physical barrier that acts like a "gatekeeper," preventing sperm from passing through the cervix into the uterus.
- Other mechanisms: Progestin suppresses endometrial growth, making it very thin and unsuitable for fertilized egg implantation. Additionally, for some users, it may partially suppress ovarian ovulation function.
Comparison of Different IUD Types (Copper vs. Hormonal)
To help you better understand the differences between the two types of IUDs, we've compiled the following comparison table. The choice largely depends on your expectations regarding menstrual changes, your body's response to hormones, and your personal health conditions.
Key Differences Comparison Table
| Feature | Copper IUD | Hormonal IUD (e.g., Mirena) |
|---|---|---|
| Main Component | Copper ions | Progestin (levonorgestrel) |
| Mechanism | Spermicidal, affects sperm activity, changes endometrial environment (prevents fertilization) | Thickens cervical mucus, thins endometrium, partially suppresses ovulation |
| Contraceptive Rate | High (first-year failure rate ~0.8%) | Very high (first-year failure rate ~0.2%) |
| Menstrual Flow | May increase flow, periods may be longer | Usually significantly reduces flow, some users may have light periods or amenorrhea |
| Dysmenorrhea | May worsen menstrual pain | Usually effectively reduces menstrual pain, can be used to treat primary dysmenorrhea |
| Emergency Contraception | Yes (placed within 5 days after unprotected intercourse, more than 99% effective) | No |
| Duration | Up to 10-12 years | Usually 5-8 years (depending on product) |
| Additional Benefits | None | Can treat heavy menstrual bleeding, dysmenorrhea, endometriosis-related pain, etc. |
| Hormonal Effects | No systemic hormonal effects | May have small amounts of hormone absorbed systemically, potentially causing headaches, mood changes, etc. |
Data references: World Health Organization (WHO) guidelines, Mayo Clinic, and related clinical research reports.
Advantages and Disadvantages of IUDs
Advantages
- Long-acting and reversible: Provides years of reliable contraceptive protection with one insertion. Fertility typically returns quickly after removal.
- Highly effective: Over 99% contraceptive success rate, one of the most effective reversible contraceptive methods available.
- Convenient and easy to use: No daily medication or pre-intercourse measures needed after insertion; you can almost "forget" its existence.
- Cost-effective: Although initial insertion cost is high, the annual cost when averaged out is very low.
- Widely applicable: Suitable for most healthy women, including nulliparous and breastfeeding women.
- Non-hormonal option: Copper IUD provides an excellent choice for women who cannot or prefer not to use hormonal products.
- Therapeutic effects: Hormonal IUD can effectively treat heavy menstrual bleeding and dysmenorrhea while providing contraception.
Disadvantages
- No STI protection: IUD only prevents pregnancy and provides no protection against sexually transmitted infections (STIs). If there's infection risk, condoms must be used simultaneously.
- Initial discomfort: In the first weeks to months after insertion, some women may experience spotting, abdominal cramping, or menstrual pattern changes.
- Potential risks: Though extremely rare, risks include IUD expulsion, uterine perforation (during insertion), or infection (if infection was present during insertion).
- Negative menstrual effects (Copper IUD): May cause increased menstrual flow, longer periods, and worsened dysmenorrhea, which is the main reason some users choose removal.
- Hormonal side effects (Hormonal IUD): Some users may experience headaches, mood changes, acne, or breast tenderness, though these side effects usually diminish over time.
- Professional dependency: IUD insertion and removal must be performed by trained healthcare professionals.
Suitable and Contraindicated Populations
According to the World Health Organization (WHO) "Medical Eligibility Criteria for Contraceptive Use," IUD suitability and contraindications are as follows:
Suitable Candidates
- Healthy women seeking long-term, highly effective, reversible contraception.
- Women regardless of parity, as long as uterine anatomy is normal.
- Breastfeeding women (usually recommended 4-6 weeks postpartum).
- Women with estrogen contraindications (such as certain migraine patients, smokers) or intolerance (can choose copper IUD or progestin-only IUD).
- Women needing emergency contraception (copper IUD only, placed within 5 days of unprotected intercourse).
- Stable HIV-positive individuals.
Contraindications and Precautions
-
Absolute contraindications (should not use):
- Current pregnancy or suspected pregnancy.
- Current pelvic inflammatory disease (PID), gonorrhea, chlamydia, or other reproductive tract infections.
- Unexplained abnormal vaginal bleeding.
- Confirmed or highly suspected uterine or cervical cancer.
- Severely abnormal uterine cavity anatomy (such as large uterine fibroids causing cavity distortion).
- For hormonal IUD: breast cancer history or severe active liver disease.
-
Relative contraindications (require careful evaluation):
- Within 4 weeks postpartum or recent septic abortion (slightly higher risk of expulsion and perforation).
- High risk for sexually transmitted infections (screening and treatment recommended first).
IUD Insertion and Removal
Insertion Process
- Pre-insertion: Doctor takes detailed medical history, performs gynecological examination to assess uterine size, position, and health, and rules out pregnancy and infection.
- Insertion procedure: Usually completed in minutes during an office visit. You lie on the examination table, doctor uses speculum to expose cervix, disinfects, then uses a thin insertion tube to gently place the folded IUD into the correct position in the uterine cavity. After IUD deployment, doctor removes insertion tube and trims strings to appropriate length.
- Insertion sensation: Most women feel cramping similar to severe menstrual cramps, usually brief.
- Post-insertion: May have light bleeding or lower abdominal discomfort lasting hours to days. Doctor will inform you of follow-up timing (usually after first menstruation) and how to self-check strings.
Removal Process
Removal is usually simpler and faster than insertion. Doctor grasps the strings at the cervix with forceps and gently pulls outward. The IUD arms automatically fold when passing through the cervical canal for smooth removal. The process may involve mild cramping. Fertility returns immediately after removal. If strings are "missing," doctor will use ultrasound to locate IUD position and use special instruments for removal.
Common Side Effects and Risk Management
Common Side Effects
- Menstrual pattern changes: Most common side effect. Copper IUD often increases menstrual flow and duration; hormonal IUD usually decreases flow and shortens periods, may even cause amenorrhea, with possible irregular spotting initially.
- Pain or discomfort: Lower abdominal cramping and back pain are common initially, usually resolving gradually within weeks to months.
Potential Risks and Complications
- Expulsion: IUD may be partially or completely expelled by the uterus, occurring in about 2-10% of cases.
- Uterine perforation: Very rare complication (incidence ~1/1000) where IUD penetrates uterine wall during insertion.
- Pelvic inflammatory disease (PID): IUD insertion itself doesn't cause PID, but may increase risk of ascending infection if undetected sexually transmitted infections (like chlamydia) are present during insertion.
- Ectopic pregnancy: IUD effectively prevents all types of pregnancy, including ectopic pregnancy. Therefore, women using IUDs have much lower absolute risk of ectopic pregnancy than women using no contraception. However, if pregnancy occurs while using an IUD, the likelihood of it being ectopic is relatively higher.
When to Seek Medical Help
Contact your doctor immediately if you experience any of the following while using an IUD:
- Suspected pregnancy.
- Persistent or worsening severe abdominal pain.
- Abnormally heavy menstrual bleeding or heavy bleeding between periods.
- Fever or abnormal vaginal discharge with odor or unusual color.
- Pain during intercourse.
- Feeling that IUD strings have become longer, shorter, or completely undetectable.
🔍 Deep Dive: Troubleshooting & Long-Term Care
IUDs are great, but they come with unique nuances. We have created specific guides for common "Taboo" or technical questions:
- Emotional Side Effects: The Mirena Crash: Why You Feel Crazy After Removal
- Nutrition: Copper IUDs & Zinc Deficiency: The Hidden Link to Anxiety
- Self-Care: How to Find Your Strings (Visual Guide)
Frequently Asked Questions (FAQ)
Q: Is IUD insertion painful? A: Pain varies among individuals. Most experience brief, severe menstrual cramp-like pain. The process is quick and discomfort usually subsides rapidly. Doctors may recommend taking pain medication before insertion.
Q: How do I choose the right IUD for me? A: This is a personalized decision to make with your doctor. If you have heavy periods or severe dysmenorrhea, hormonal IUD might be better. If you want to avoid hormones or need ultra-long-term contraception, copper IUD might be more suitable.
Q: How long does an IUD last? Does it need regular replacement? A: Each IUD type has a specific effective period (5-12 years). You need to have it removed when it expires. If you want to continue contraception, a new one can be inserted immediately.
Q: How soon can I get pregnant after IUD removal? A: Fertility returns quickly. Theoretically, you can try to conceive in the next ovulation cycle after removal.
Q: How soon can I have intercourse after IUD insertion? A: Most doctors recommend waiting 24 hours or until initial bleeding and discomfort subside before resuming sexual activity.
Q: Will my partner and I feel the IUD during intercourse? A: You shouldn't feel the IUD itself. Your partner might feel the soft strings at the top of the vagina, but this usually doesn't cause discomfort. If strings are too long and bothersome, ask your doctor to trim them.
Conclusion
The intrauterine device (IUD) is a safe, highly effective, and extremely convenient long-acting reversible contraceptive choice for modern women. It comes in two main types—copper and hormonal—each with unique advantages and suitable scenarios. Under professional healthcare provider operation, insertion and removal procedures are usually safe and simple. While there are some common initial side effects and extremely rare risks, through proper selection, regular follow-up, and timely communication, the vast majority of women can benefit from IUDs.
Remember, choosing the most suitable contraceptive method is an important personal decision. Before making a choice, having a thorough, honest conversation with your doctor is crucial.
References
- World Health Organization (WHO). (2015). Medical eligibility criteria for contraceptive use (5th ed.).
- American College of Obstetricians and Gynecologists (ACOG). (2021). Practice Bulletin No. 186: Long-Acting Reversible Contraception: Implants and Intrauterine Devices.
- NHS (National Health Service, UK). (2022). Intrauterine device (IUD).
- Mayo Clinic Staff. Intrauterine device (IUD). Mayo Clinic.
This content is for educational and informational purposes only and should not replace professional medical advice, diagnosis, or treatment. If you have health concerns, please consult healthcare professionals.
Quick Actions
⚠️ Medical Disclaimer
This content is for educational and informational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. If you have any health concerns or questions, please consult a qualified healthcare professional. Always seek the advice of your physician before making any health-related decisions.
📚 Related Articles
Continue exploring more professional health content
More Articles Coming Soon
We are preparing more high-quality health content, stay tuned.
Browse All Articles